Abstract
Introduction:
Multiple myeloma (MM) and Waldenström's macroglobulinemia (WM) are related plasma cell disorders that respond to treatment with proteasome inhibitors. Several early phase studies have shown that carfilzomib (Cz) is highly effective as the initial treatment of MM and results in deep remissions in most patients. A randomized phase III study is evaluating the efficacy of Cz or bortezomib with lenalidomide and dexamethasone as frontline therapy in MM and could lead to changes in the treatment of choice (NCT01863550). A clinical trial also showed good tolerance and efficacy of Cz in the frontline treatment of WM. In this study we aim to report the efficacy and safety of frontline Cz-based combinations in MM and WM in a standard of care setting.
Methods:
In this retrospective, single center study, we queried our ambulatory and inpatient (IPATC) database to identify subjects who were diagnosed with MM or WM and received Cz as initial therapy from 4/1/2014 to 11/30/2016. Investigational Cz was excluded. We identified 54 patients with MM (including one with concurrent lambda AL amyloidosis) and 6 patients with WM. Responses were assessed based on guidelines published by the International Myeloma Working Group (Kumar et al. Lancet 2016) and the VI international workshop on WM (Owen et al. BJH 2013). The Kaplan-Meier method was used to estimate time-to-event endpoints including progression free survival (PFS). Statistical software SAS 9.3 (SAS, Cary, NC) and S-Plus 8.2 (TIBCO Software Inc., Palo Alto, CA) were used for all the analyses.
Results:
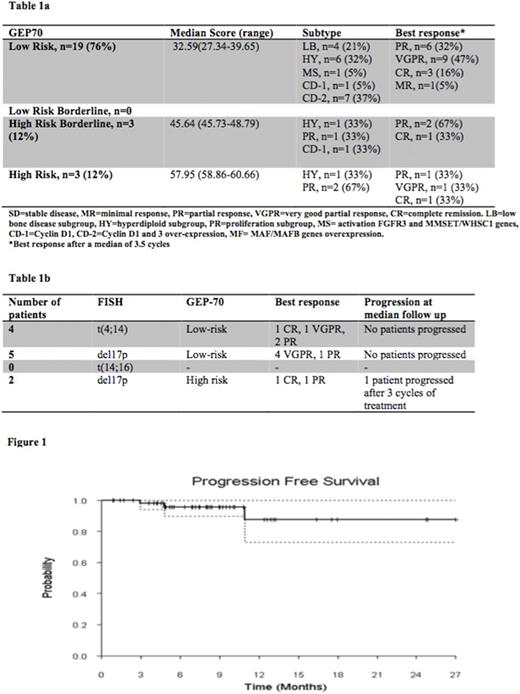
All MM patients were treated with either KRd (Cz, lenalidomide, dexamethasone) (n=52, 96%) or KCd (Cz, cyclophosphamide and dexamethasone) (n=2, 4%). Median age at diagnosis was 66 years (range 60-70 years). Revised International Staging System (R-ISS) stage I, II or III was present in 20 (37%), 28 (52%) and 6 (11%) patients, respectively. Patients presented with either CRAB criteria (n=48, 89%) or biomarkers of malignancy (n=4, 7%) and 22% had extramedullary disease. Gene expression profiling-70 (GEP-70, Quest Diagnostics) was available for 25 patients (Table 1a). Patients with both high-risk GEP and FISH had early relapse (Table 1b). The maximum doses of Cz used were 36 mg/m2 (n=44), 27 mg/m2 (n=6) and not available (n=4). After a median of 3 cycles, eligible patients underwent autologous stem cell transplant (ASCT) (n= 36, 77%). Fifty-two patients were evaluable for response. After a median of 3 cycles of initial treatment, overall response (ORR) was 98% [complete remission (CR; n=9, 17%), very good partial response (VGPR; n=27, 52%) and partial response (PR; n=15, 29%)]. After ASCT, responses deepened to CR (n=18, 50%), VGPR (n=9, 25%) and PR (n=4, 11%). Eleven patients did not undergo ASCT (comorbidities: 6, insurance issues: 1, patient preference: 3, progression: 1). The median number of cycles received in this group was 4 and best responses were CR (n=3, 30%), VGPR (n=2, 20%), PR (n=5, 50%) while 1 not evaluable. At a median follow up of 7.4 months, overall survival (OS) is 100% while median PFS has not been reached (Figure 1). Five patients discontinued therapy due to toxicity (one of each with pericarditis, shortness of breath, pulmonary toxicity, neuropathy, retroperitoneal bleeding) and 3 due to progressive disease. There were no reported cases of heart failure.
Patients with WM, n=6, [MYD88 mutation positive (n=5, 83%), CXCR4 mutation positive (n=0)] were treated with Cz, rituximab and dexamethasone induction followed by maintenance as described by Treon et al. (Blood 2014). Median age was 57 years (range 52-74 years). Patients presented with B symptoms (n=6, 100%) and anemia (n=5, 83%). After a median of 6 cycles of therapy, ORR was 66% [CR: n=1 (17%), PR: n=3 (50%)] while 2 (33%) had minimal response. All patients had resolution of B symptoms and anemia after treatment. One patient (MYD88 positive, CXCR4 negative) relapsed 27 months after starting initial treatment. Only one patient had severe toxicity (debilitating neuropathy attributed to rituximab) prompting therapy discontinuation after 3 cycles (Alfaraj et al, Ann Hematol. 2016). At a median follow up of 33.5 months, OS is 100%. Mutational status did not seem to impact response to therapy.
Conclusion:
Cz based regimens are generally well tolerated and offer a neuropathy sparing approach with excellent responses in newly diagnosed MM and WM making them a good choice for frontline treatment of these diseases.
Lee: Celgene: Consultancy; Eutropics Pharmaceuticals: Research Funding; Adaptive: Membership on an entity's Board of Directors or advisory committees; Pimera Inc: Consultancy; Daiichi Sankyo: Research Funding; Takeda: Consultancy. Orlowski: BioTheryX: Consultancy, Membership on an entity's Board of Directors or advisory committees. Manasanch: quest diagnostics: Research Funding; merck: Research Funding; celgene: Consultancy; takeda: Consultancy; sanofi: Research Funding; adaptive biotechnologies: Consultancy.
Author notes
Asterisk with author names denotes non-ASH members.

This feature is available to Subscribers Only
Sign In or Create an Account Close Modal